Medication errors harm an estimated 1.3 million people annually and cause a death per day in the United States, according to the World Health Organization. In busy hospitals, the cause may be as routine as an interruption—a doctor asking the administering nurse for information or a colleague wanting to chat during the process of assembling the right medications and dosages for a patient. Studies have indicated that interruption rates may be as high as 94.5% during medication administration. But interruptions seldom are part of student nursing education.
Now Temple is participating in a multi-site study aimed at creating effective ways to train pre-licensure nursing students to manage interruptions in clinical settings. Temple has joined with Loyola University Chicago, the University of Kansas and the University of Illinois at Chicago to conduct a series of simulations testing a methodology for teaching interruption preparedness during medication administration and nurse to nurse handoff. The study is funded by the National League for Nursing, which promotes nursing education, in part via research grants.
"Nobody is really teaching this at the pre-licensure level. They'll teach it when they get into the hospital when they're new nurses,” says Susan Kilroy, assistant professor of instruction and director of Temple’s Nursing Simulation Lab. “The goal is to eventually include it in our nursing curriculum.”
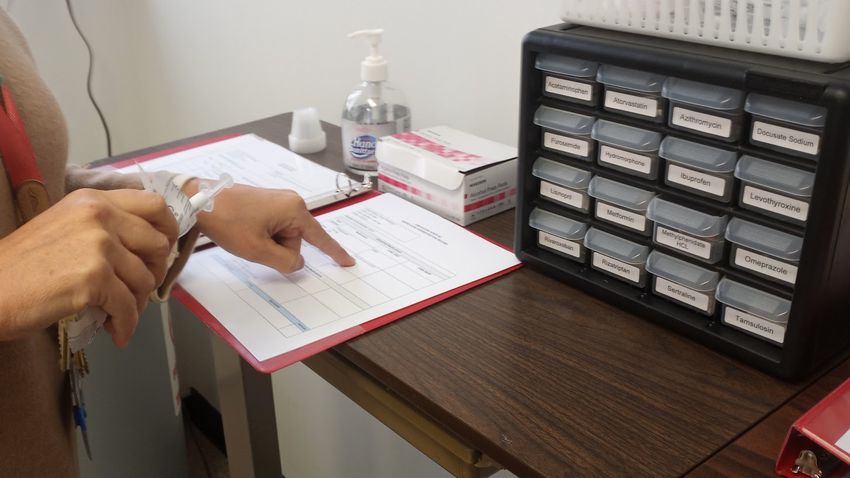
The Nursing Simulation Lab, located at Temple’s Health Sciences Campus, includes a simulated hospital room with a manikin in the bed and a second room with a medication dispensary station. Temple student nurses, as subjects of this study, each run through the same patient scenario. First, the nurse enters the patient room to receive morning report. Kilroy gives the incoming nurse a specific set of information utilizing a method called SBAR, for Situation-Background-Assessment-Recommendation, which includes patient information reported in an organized fashion. The nurse then goes to the medication room with the patient chart to obtain the correct medications—and is interrupted while doing so.
The study puts each student nurse through three sessions, separated by several weeks, that represent increasing levels of interruption. The first time, it’s a charge nurse making friendly conversation. In the second session, it’s a doctor interrupting to ask for patient information. The third session’s interruption is an emergency situation, “and the doctor is stressed,” Kilroy says.
On a recent afternoon, enacting the second scenario, clinical nursing instructor Brenda Teichman portrays “Dr. Lee,” interrupting nursing students while they are collecting medications. Following a script used by all of the study sites, she says she is in a hurry and asks the busy nurse for an overview of the patient’s condition. Two Temple nursing graduates, Stephanie Scoma ’23 and Elvin Luna '18, are also working on the research project as embedded charge nurses/doctors.
Students learn to handle the stress and distraction of each scenario. Although computerized medication dispensing systems have cut errors, nurses still must concentrate on the task of getting each patient the correct meds. A nurse may need to keep a finger pressed down to mark a particular place in a patient chart while answering questions, or ask the interrupter about the urgency of the situation, or raise a hand to silence someone who’s trying to interrupt, Kilroy says.
After gathering the meds, the student nurses return to the patient room to administer the medication—in this scenario, it’s oral medicine and an injection. They need to follow standard protocols for administering the medications, including washing hands, putting on gloves, checking the patient’s wristband, and talking with the patient. In a nearby control room, Kilroy watches the nurse-patient interaction on a video monitor and speaks through a headset to converse with the nurse as the recovering patient.
In the control room, Kilroy and Teichman discuss each nurse’s performance and fill out a checklist, while students fill out a self -reflection. Then Kilroy returns to the patient room to discuss with the student how it went and offer guidance for improvements, and they repeat the procedure, which is also called deliberate practice. “We do it again at bedside, a shortened version, because then it solidifies. They can correct all the things we’ve just talked about,” she says.
At the end, there’s a final debriefing and evaluation. “We want to hear how they feel during the simulations and how they are processing the information,” Kilroy says.
Nursing students do have clinical hours working with real patients, but real-life settings are not the ideal place to learn from trial and error. The results from Temple and the other study sites will help identify how simulation training for interruption management can be worked into more nursing curricula.
“A sim is where you can make mistakes and learn,” Kilroy says. “The idea is, the first time, they come and make mistakes, and that’s okay, and they do the education and deliberate practice. The second time, they get a little better. And then the third time, they have the confidence to implement the skills they learned and it’s like, ‘OK, I’ve got this.’”
