The bird flu outbreak in the United States continues to impact poultry, dairy cows, and humans, creating widespread concerns for public health and the agricultural industry.
What Is Bird Flu?
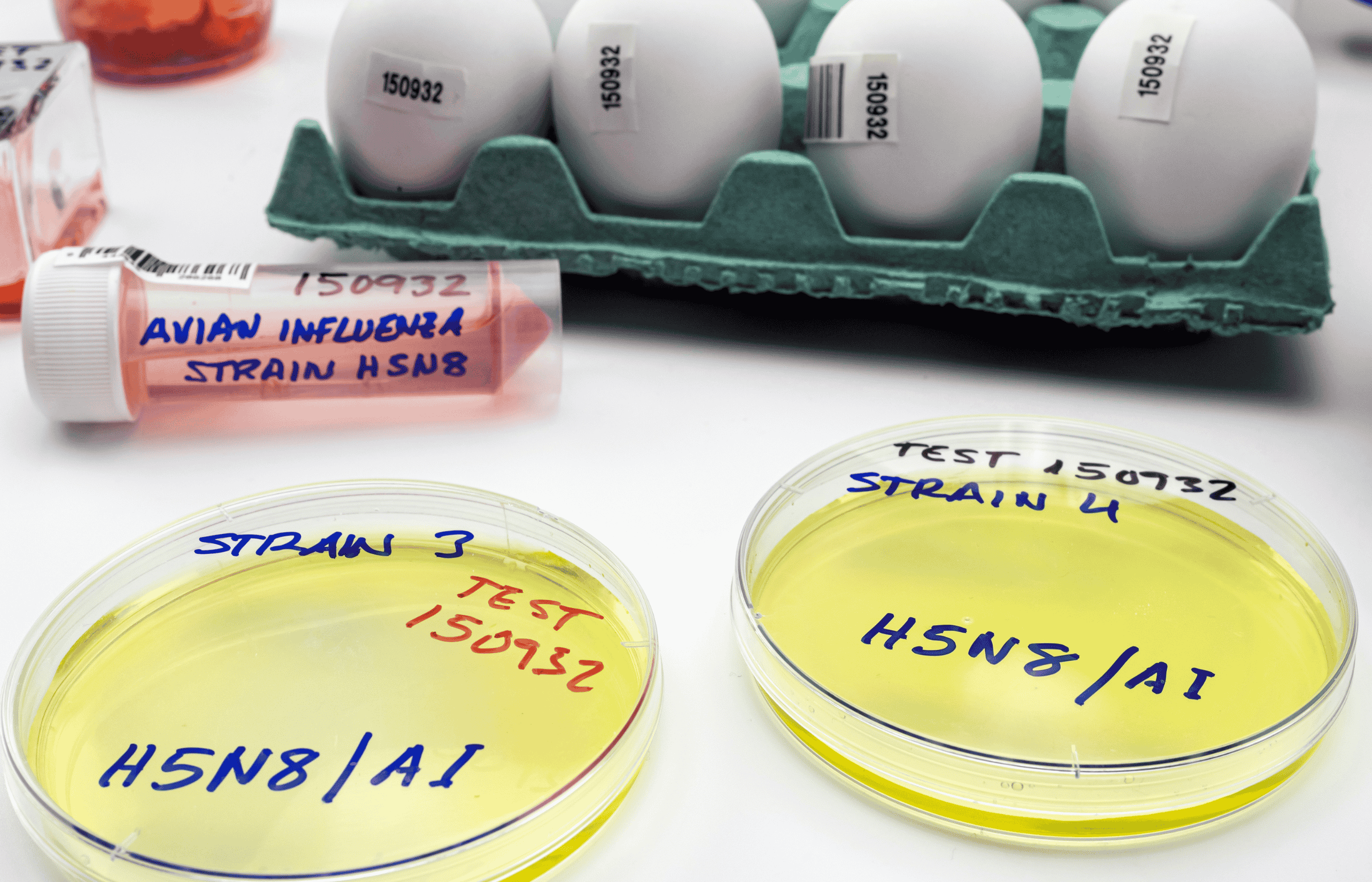
Bird flu, or avian influenza, is a viral infection that primarily affects wild birds but can spread to domestic poultry and other animals, including humans. The H5N1 strain, responsible for the current outbreak, is highly pathogenic, causing severe illness and death in birds. It spreads through direct contact with infected animals, their droppings, or contaminated environments (CDC, 2024).
While human infections are rare, they can occur when people are exposed to sick birds, infected mammals, or contaminated products. Symptoms in humans range from mild respiratory issues to severe illness, and in rare cases, death (WHO, 2024). The virus’s ability to infect new hosts, including mammals like cows and cats, has heightened concerns about its potential to adapt for human-to-human transmission.
According to Dr. Kirsten Wiens, an infectious disease epidemiologist at Temple University, while mutations that allow H5N1 to infect humans are becoming more common, those enabling sustained human-to-human transmission remain much less likely. "What makes this outbreak concerning is the virus’s continued spread in poultry and its unprecedented spillover into dairy cows. The more the virus replicates, the greater the chance that a mutation could emerge, increasing the risk of human transmission," she explains.
Human Cases
The United States reported its first human case of H5N1 avian influenza in two years in April 2024. Since then, 67 infections have been confirmed, most of them mild (CDC, 2024). However, the first U.S. death from bird flu was recorded this month in Louisiana (Louisiana Department of Health, 2024).
The majority of human cases are linked to exposure to sick dairy cows or poultry. While pasteurization effectively eliminates the virus in milk, raw milk remains a significant risk factor (FDA, 2024). Poultry workers involved in culling operations have also been infected, and a small number of cases have yet to be traced to a definitive source. The Centers for Disease Control and Prevention (CDC) has emphasized that there is no evidence of human-to-human transmission (CDC, 2024).
Dr. Wiens highlights that human cases are typically detected through nasal or throat swabs, which accurately confirm H5N1 if collected within a few days of symptom onset. "Since many infections cause similar symptoms, testing is typically prioritized for high-risk exposures," she notes. The CDC and local health departments actively monitor individuals exposed to infected birds, poultry, and dairy cows to prevent misdiagnosis and delayed detection (CDC, 2024).
Impact on Poultry and Cat Cases
The outbreak continues to devastate poultry farms nationwide, with recent infections reported at broiler farms in Georgia, Maryland, and Virginia, an egg farm in Missouri, and a duck farm on Long Island, New York (USDA, 2024). Avian influenza is so lethal in poultry that entire flocks are culled as soon as infections are confirmed, contributing to rising egg prices. Since the outbreak began in February 2022, over 140 million birds have been infected or culled (CIDRAP). While cooked poultry and eggs are safe to consume, raw or undercooked eggs should be avoided due to the risk of pathogens.
Domestic cats have also emerged as unexpected victims of the H5N1 virus, with cases confirmed in California, Kansas, Louisiana, and Iowa this January, along with additional infections from December (AVMA, 2024). Cats on dairy farms are particularly vulnerable, likely due to consuming raw milk from infected cows. Outdoor cats may contract the virus from wild birds, while indoor cats face risks from contaminated raw pet food.
Dr. Wiens explains why dairy cows and domestic cats are particularly susceptible: "Dairy cows, which often spend time outdoors, can be exposed to infected birds and may also contract the virus through contaminated equipment, such as milking machines. Cats may ingest contaminated food or come into contact with infected wild birds." The fact that H5N1 is infecting new mammalian hosts suggests the virus is adapting, though it remains unclear how efficiently it can spread between them.
In response to the growing threat, the Food and Drug Administration (FDA) issued a mandate on January 17 requiring raw pet food manufacturers to update their food safety plans to address H5N1 contamination.
Response Challenges
The spread of H5N1 among wild birds, poultry, and cows complicates monitoring efforts. Human cases are managed by state health departments with CDC coordination, while agricultural outbreaks fall under the U.S. Department of Agriculture (USDA). The recent communication freeze ordered by President Donald Trump has created challenges for federal coordination and transparency (Reuters, 2025).
Coordination challenges between agencies can slow outbreak response, delay resource allocation, and lead to conflicting or unclear public messaging, warns Dr. Wiens. "Efficient communication is essential for timely containment and public awareness."
Protective Measures
To minimize exposure risks, Dr. Wiens advises poultry workers and dairy farmers to wear protective equipment like gloves, goggles, and face masks, especially in high-risk settings. "They should also frequently wash their hands and disinfect potentially contaminated surfaces," she adds.
Pet owners should take precautions as well. "Ensure that any poultry or dairy products your pets consume are fully cooked and pasteurized. Prevent pets from interacting with wild birds," Dr. Wiens recommends.
Additionally, she emphasizes the importance of flu vaccinations. "While the flu shot won’t prevent bird flu, it reduces the risk of seasonal influenza and helps healthcare workers focus on potential bird flu cases."
Looking Ahead
In the past 30 days, over 100 infected poultry flocks have been reported, impacting over 15 million birds, according to the USDA. The virus’s adaptation to new hosts—ranging from cows to humans—raises concerns about mutations that could increase human transmission. Scientists emphasize the importance of pasteurization, avoiding raw eggs, and adhering to biosecurity measures to minimize risks.
While sustained human-to-human transmission remains unlikely, the continued spread of H5N1 in new mammalian hosts draws attention to the need for continued vigilance, research, and a coordinated public health response.